10 Facts About Back Pain
This infographic highlights 10 key facts about back pain that both patients and therapists can benefit from.

The cornerstone of successful management of LBP is patient education. There is level 1 evidence that educating patients provides reassurance which in turn reduces fear, anxiety and pain related distress [1]. As primary care practitioners, physiotherapists have the opportunity to provide long lasting reassurance to patients with LBP through structured and timely education. The well established correlation between stress and pain sensitization [2], implicates that reassurance alone can have a concomitant positive impact on an individuals pain, disability and recovery.
This systematic review illustrates the efficacy of reassurance in reducing pain-related distress in acute and chronic LBP.
Providing an accurate evidence-based prognosis to individuals with LBP, is an essential component of delivering education that instills long lasting reassurance.
This ground breaking systematic review demonstrates that a majority of cases of LBP will improve over 6 weeks regardless of the treatment given [3]. This has important implications for the way physiotherapists approach management of both acute and chronic presentations of LBP. Empowering patients with an accurate knowledge of prognosis should be a first line intervention in itself utilized in every case of LBP.
The Body-Mind Interaction in Low Back Pain

In this article, Dr Mary O’Keffe and Dr Kieran O’sullivan challenge some widely held myths about LBP. They highlight the under-emphasized importance of sleep, general health and psychological contributors of LBP.
Back Pain: Separating Fact From Fiction
This impactful video by Pain-Ed, is a powerful reminder that education alone can change an individual’s beliefs about their back pain which can ultimately lead to radical changes in their pain experience and disability.
An often overlooked contributor to low back pain, sleep is a modifiable lifestyle factor that can cause, prolong and exacerbate acute and chronic low back pain.
The infographic below provides a summary of an article by Pain-Ed on the relationship between sleep and low back pain.

- Discs can heal
This entertaining blog post by Jarod Hall, delves into the evidence on the ability of intervertebral discs to heal.
The article highlights the overwhelming amount of literature affirming that asymptomatic intervertebral disc injuries are common and can heal [1],[2].
This information is not emphasized enough in a majority of the undergraduate and graduate physiotherapy curriculum’s. We believe this has contributed to the pervading belief of the frailty of discs among patients and health care providers.
Full credit to Jarod Hall for providing this blog post. Jarod’s blog has a multitude of educational posts for physiotherapists and can be found here.
2. Discs Don’t ‘Slip’
If you have ever had difficulty explaining to a patient the pathophysiology, prevalence and prognosis of a disc injury, then read on.

Physio Network have recently published an informative blog post written by Jarod Hall on this very topic. The article is well worth pursuing as it will undoubtedly help you be more accurate, encouraging and purposeful in the language you use and manner in which you explain disc-related low back pain to patients.
Full access to the blog post can be found here.
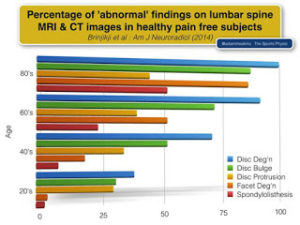
3. Back pain is not solely due to changes in disc shape or structure
In this convincing, research based article, the team at Pain-Ed explain why the infamous disc cannot be blamed as the only cause of back pain and propose a holistic approach to management.
Scans for low back pain fact sheet
NPS MedicineWise published a recent educational handout for patients simplifying the role of imaging for low back pain [1].
Additional useful resources from NPS Medicinewise on LBP for both patients and clinicians can be found here.
ABC Podcast ‘Wasteful Scans in Low Back Pain’
A short 10 minute interview with Dr Richard Deyo on imaging for low back pain.
- Traeger, A. C., Hübscher, M., Henschke, N., Moseley, G., Lee, H., & McAuley, J. H. (2015). Effect of primary care–based education on reassurance in patients with acute low back pain: Systematic review and meta-analysis. JAMA Intern Med, 175(5), 733-743. doi:10.1001/jamainternmed.2015.0217
- Caneiro, J. P., O’Sullivan, P., Smith, A., Moseley, G. L., & Lipp, O. V. (2017). Implicit evaluations and physiological threat responses in people with persistent low back pain and fear of bending. Scandinavian Journal of Pain, 17, 355-366. doi:https://doi.org/10.1016/j.sjpain.2017.09.012
- da C Menezes Costa, L., Maher, C. G., Hancock, M. J., McAuley, J. H., Herbert, R. D., & Costa, L. O. P. (2012). The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 184(11), E613-E624. doi:10.1503/cmaj.111271
- Brinjikji, W., Luetmer, P. H., Comstock, B., Bresnahan, B. W., Chen, L. E., Deyo, R. A., . . . Jarvik, J. G. (2015). Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR. American journal of neuroradiology, 36(4), 811-816. doi:10.3174/ajnr.A4173
- Chiu, C.-C., Chuang, T.-Y., Chang, K.-H., Wu, C.-H., Lin, P.-W., & Hsu, W.-Y. (2015). The probability of spontaneous regression of lumbar herniated disc: a systematic review. Clinical Rehabilitation, 29(2), 184-195.
- NPS MedicineWise (2018, October, 2018). Low back pain: Do you need a scan? Retrieved from https://www.nps.org.au/medical-info/clinical-topics/low-back-pain#resources