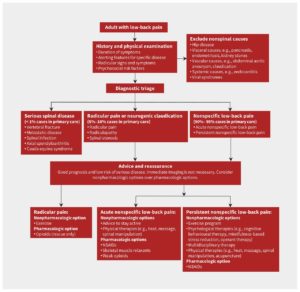
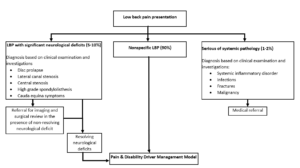
The diagram below provides a simple diagnostic and management guideline that should be used in all cases of low back pain. It is based on current clinical practice guidelines from the United Kingdom and United States [1].
| (Traeger, Buchbinder, Harris, & Maher, 2017) |
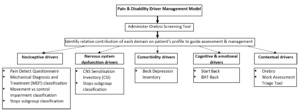
As with all musculoskeletal presentations, evidence based management of LBP involves recognizing the multitude of factors contributing to an individual’s symptoms [2].
These may include:
- Movement/motor control dysfunctions: repetitive movements, sustained postures, excessive bracing, dysfunctional lumbopelvic and/or diaphragmatic control.
- Sensitization of spinal structures: caused by neuro-immune endocrine system maladaptation.
- Psychological factors: anxiety, poor self efficacy, low mood, fear avoidance, damage beliefs.
- Lifestyle/health behaviours: insufficient sleep and recovery, inactivity, high stress, smoking/drinking, poor dietary habits.
- Genetic factors: family members with LBP, family history of arthritis.
Evidence indicates that in both acute and chronic cases of LBP, the primary factors driving pain and disability are often related to an individual’s illness perceptions and behavioral coping responses to pain rather than structural pathology and tissue damage [3].
A recent longitudinal study by Glattacker, 2018 investigated the contribution that psychosocial factors have as predictors of rehabilitation outcomes in individuals with chronic low back pain (CLBP).
What they found was that a combination of a better work prognosis, self-efficacy and intensity of depressive symptoms were verified as independently significant predictors of quality of life outcomes in individuals with CLBP within a rehabilitation setting. The study highlights that psychosocial factors may implicate poor recovery and/or a high risk of developing chronic symptoms [4].

The majority of LBP cases resolve before physiologically accepted tissue healing time frames. Indicating that the primary nociceptive drivers of many LBP cases are multifactorial and not purely biomechanical [3, 5].
There are certainly cases of LBP where mechanical factors are the primary drivers of pain and should be addressed. However, true neurological comprimise and lumbrosacral radiculopathy, represent just 1-2% of all presentations [5].
The prevailing belief among patients and clinicians that LBP is predominately caused by damage/injury to structures in the back, is misguided [5].
CLINICAL REASONING FRAMEWORK
The challenge for physiotherapists is to identify the primary factors contributing towards their pain and disability. Below is a framework designed to assist with this process.
RADAR GRAPH
Following a subjective and objective assessment, the following form can be quickly utilized by the therapist to create a visual representation of the relative contribution of each domain driving a patient’s pain.
This may be beneficial for the therapists’s clinical reasoning and as a visual education tool for patients.
WHEN TO USE IT:
The MyBack self assessment tool is a validated prognostic screening tool for patients with actue LBP. It can be used by patients or clinicians to help identify the severity of LBP and risk of serious pathology. The resource can be administered in an initial assessment to guide your clinical decision making.
INTERPRETING RESULTS:
This tool has a high sensitivity and can result in false positives. As highlighted in the red flags section of this resource, the best indicator of a serious underlying pathology, is a cluster of accurate red flags. Simply having one red flag (e.g. night pain) in isolation is not considered an accurate indication of serious underlying pathology. If ever in doubt, seek a second opinion from a senior colleague or trusted general practitioner.

Learn more here.
| Screening tool/ questionnaire | Suggested use |
|---|---|
| Pain Detect Questionnaire | An objective diagnostic tool to distinguish the dominance of nociceptive and neuropathic pain |
| CNS Sensitization Inventory (CSI) | Assists in identifying the presence of central sensitization and CNS sensitization syndromes |
| Beck Depression Inventory | Screening tool for depression |
| STarT Back Tool | Identify modifiable risk factors (biomedical, psychological and social) for back pain disability |
| Behavioral Avoidance Test-Back | A validated Behavioral Avoidance Test (BAT) for chronic low back pain (CLBP) patients assessing pain-related avoidance behavior through direct observation. |
| Örebro Musculoskeletal Pain Questionnaire (ÖMPQ) | Screening questionnaire for psychosocial risk factors (multifactorial persistent pain) |
| Work Assessment Triage Tool | Developed to enable clinicians to select optimal rehabilitation treatment options for injured workers with musculoskeletal conditions |
| The PICKUP tool | Developed to predict persistent pain in patients with a recent onset of low back pain. |
The Clinical Edge website provides valuable video resources on how to conduct a general objective examination of a LBP presentation.
These resources will help you refine your clinical testing.
- Traeger, A., Buchbinder, R., Harris, I., & Maher, C. (2017). Diagnosis and management of low-back pain in primary care. Cmaj, 189(45), E1386-e1395. doi:10.1503/cmaj.170527
- Tousignant-Laflamme, Y., Martel, M. O., Joshi, A. B., & Cook, C. E. (2017). Rehabilitation management of low back pain – it’s time to pull it all together! Journal of Pain Research, 10, 2373-2385. doi:10.2147/JPR.S146485
- Rabey, M., Smith, A., Beales, D., Slater, H., & O’Sullivan, P. (2016). Differing Psychologically Derived Clusters in People With Chronic Low Back Pain are Associated With Different Multidimensional Profiles. Clin J Pain, 32(12), 1015-1027. doi:10.1097/ajp.0000000000000363
- Glattacker, M., Heyduck, K., & Jakob, T. (2018). Yellow flags as predictors of rehabilitation outcome in chronic low back pain. Rehabilitation Psychology, 63(3), 408-417. doi:10.1037/rep0000200Glattacker, M., Heyduck, K., & Jakob, T. (2018). Yellow flags as predictors of rehabilitation outcome in chronic low back pain. Rehabilitation Psychology, 63(3), 408-417. doi:10.1037/rep0000200
- O’Sullivan, P. B., Caneiro, J. P., O’Keeffe, M., Smith, A., Dankaerts, W., Fersum, K., & O’Sullivan, K. (2018). Cognitive Functional Therapy: An Integrated Behavioral Approach for the Targeted Management of Disabling Low Back Pain. Physical therapy, 98(5), 408-423. doi:10.1093/ptj/pzy022